According to a new report, a woman with COVID-19 in Washington shed infectious virus particles for 70 days. That is, it was contagious all the time, even though there were no symptoms of the disease.
71 year old woman leukemia, Or white blood cell cancer, and she Immune system It has weakened and is unable to remove the new coronavirus known as SARS-CoV-2 from the body. Researchers suspect that people with weakened immunity may release the virus longer than usual, but there has been little evidence that this is happening.
The findings are inconsistent with the guidelines from Centers for Disease Control and Prevention (CDC) states that people with COVID-19 immunodeficiency are likely not infectious after 20 days.
New findings suggest that “long-term release of the infectious virus may be a concern for certain immunocompromised patients,” the authors journaled Wednesday (November 4). I wrote in the paper published in. cell..
“If the virus continues to spread, it will infect people with a variety of immunosuppressive disorders. It is important to understand how SARS-CoV-2 behaves in these populations,” he said. Senior author Vincent Munster, a virologist at the National Laboratory, is studying. Allergies and infectious diseases, Said in a statement..
Relation: 14 coronavirus myths destroyed by science
Unusual case
The woman was infected in late February during the country’s first reported outbreak of COVID-19 at a life care center rehabilitation facility in Kirkland, Washington, where she was a patient.
She was hospitalized for cancer-related anemia on February 25, and as she came from the center with the outbreak, doctors screened her for COVID-19. She tested positive on March 2nd.
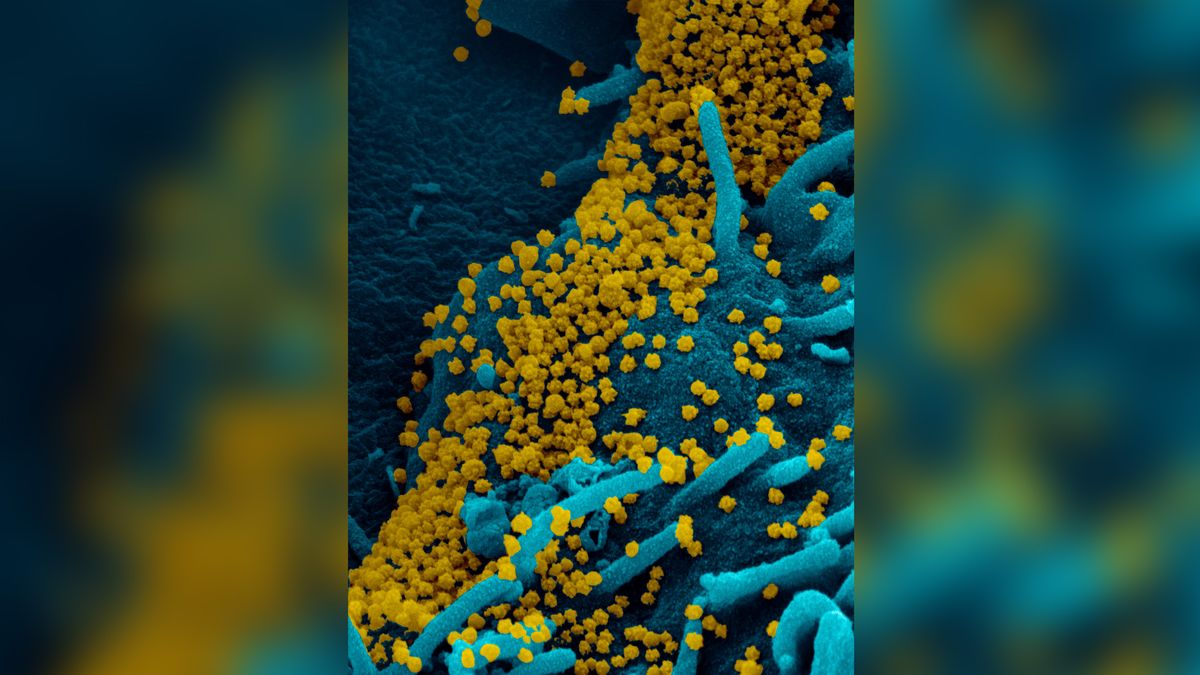
Over the next 15 weeks, women will be tested for COVID-19 more than 12 times. The virus was detected in her upper respiratory tract for 105 days. Infectious virus particles (that is, capable of spreading the disease) were detected for at least 70 days. Specifically, researchers were able to isolate the virus from a patient’s sample and propagate it in the laboratory. They could even capture images of the virus using scanning and transmission electron microscopy.
According to the report, people with COVID-19 are usually infected for about 8 days after infection. Previously, the maximum duration of infectious viral shedding in COVID-19 patients was reported to be 20 days.
The woman was probably contagious for a long time because her body did not initiate a proper immune response.Indeed, it didn’t seem to be included in the female blood sample antibody Against the virus.
The woman received two rounds of treatment Convalescent plasma, Or blood from recovered COVID-19 patients containing antibodies against the disease. She cleared the infection after the second treatment, but the woman’s antibody levels are still low after the transfusion, so there is no way to tell if convalescent plasma is effective.
The authors also sequenced SARS-CoV-2 during the female infection process and confirmed that the virus develops several mutations over time. However, the mutation did not affect the replication rate of the virus. Moreover, the authors did not see evidence that any of these mutations provided a survival benefit to the virus. This is because none of the mutated variants became predominant in the process of infection.
Unsolved mystery
The exact way women cleared the virus is unknown and needs to be considered in future studies of patients with weakened immune systems, the authors said.
Moreover, researchers do not know why women have never experienced it. Symptoms of COVID-19 Despite being immunocompromised, she is at increased risk of serious illness, According to the CDC..
“You will certainly think that immunodeficiency can spread the virus from the upper respiratory tract (a more common cold scenario) to the lower respiratory tract (pneumonia),” Münster told live science by email. Told. “The patient had been infected for at least 105 days, but this obviously didn’t happen, so this remains a mystery to us.”
The authors state that this finding does not necessarily apply to all patients with an immune system-suppressing condition, as their study included only a single case.
An estimated 3 million people in the United States are immunocompromised. HIV, The authors said, as well as those who received stem cell transplants, organ transplants, and chemotherapy.
“Understanding the mechanism of virus persistence and final clearance [in immunocompromised patients] It is essential to provide adequate treatment and prevent SARS-CoV-2 infection, “the authors conclude.
Originally published in Live Science.