Five patients with difficult-to-treat lupus went into remission after scientists fine-tuned immune cells using techniques commonly used to treat cancer. of patients with autoimmune disease discontinued standard therapy and have not relapsed.
Known as chimeric antigen receptor (CAR) T-cell therapy, this treatment needs to be tested in a larger group of lupus patients before it is approved for widespread use. If maintained in meaningful trials, this treatment may one day offer relief to people with moderate to severe lupus.
Dr. Georg Schett, Director of Rheumatology and Immunology, Friedrich-Alexander University Erlangen-Nuremberg, Germany, said: Shett is the senior author of a new report describing a small trial published Thursday (September 15) in the journal. natural medicine (opens in new tab).
“This is a single injection of CAR T cells and the patient stops all treatment,” Schett told Live Science. “We were really surprised [at] How good is this effect? ”
Related: Scientists Finally Prove There Are Mysterious Immune Cells Inside Humans
immune system reboot
Lupus is a chronic disease that immune system It inadvertently attacks the body’s own cells, causing inflammation, tissue damage, pain, and fatigue. Symptoms range from mild to life-threatening and can manifest as “flares,” and patients frequently take multiple medications to reduce their frequency and severity.
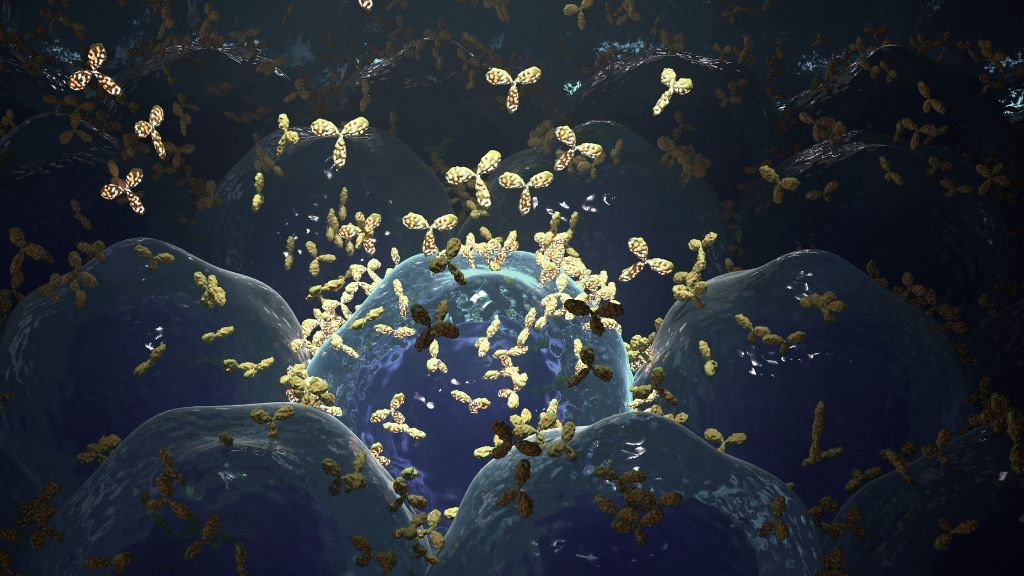
In lupus, dysfunctional B cells, a type of immune cell, send out “autoantibodies” that glome into the body’s cells and summon other cells to destroy them. Although some drugs target these harmful B cells, they do not work for all lupus patients.
“There’s a very severe group that repeats several treatments and never goes into remission,” Shett said.
Schett’s group theorized that such treatment-resistant lupus patients might benefit from CAR T-cell therapies previously used for treatment. cancer Patience. Doctors extract during CAR T-cell therapy immunity Cells called T cells are taken from the patient’s blood, genetically engineered in the lab, and given back to the patient’s body. According to the NIH’s National Cancer Institute (opens in new tab) (NCI). In all approved cancer treatments, these genetically engineered T cells target B cells with specific molecules on their surface, wiping out both problem and healthy B cells.
Without these B cells, patients may be more susceptible to infections, and CAR T-cell therapy also carries the risk of causing ‘cytokine release syndrome’. Therefore, despite its potential benefits, this treatment is not suitable for people with only mild disease.
For the trial, Schett and his colleagues recruited treatment-resistant patients with the most common form of lupus called systemic lupus erythematosus (SLE). All trial participants showed damage to multiple organs, including kidneys, hearts, lungs and joints.
Related: New tool estimates your immune ‘age’ and predicts disease risk
After treatment, B-cell counts plummeted in all five participants, as did autoantibody levels. Their lupus symptoms abated and all stopped taking their previous medications.To date, no patient has relapsed. New England Journal of Medicine (opens in new tab) — Currently in 17 months of drug-free remission.
“She lives a completely normal life,” Shett said.
Notably, five months after treatment, the patient’s B-cell count began to increase, but the symptoms did not return. Her hordes of dysfunctional B cells disappeared from her body, so her bone marrow began to make new “baby” B cells. This B cell of his didn’t pump out the same autoantibodies that his predecessor did, Schett said.
Four other patients also started making new B cells within months of treatment without recurrence. By rebooting his B-cell system in this way, Schett said he could prevent the disease from recurring, but to make sure the patient continued to be monitored, Schett said.
“A follow-up of 8 months on average is too early to determine whether this is a complete remission.” Trial. “These naive B cells may re-encounter self-antigens over time and become autoreactive,” Lin told her Live Science in an email.
No patients developed cytokine release syndrome or other serious side effects, she noted, but this may not be the case for all lupus patients. However, as more patients receive treatment, more side effects may surface,” said Ronald van Volenhoven, professor of rheumatology at the University of Amsterdam Medical Center, who was not involved in the trial. PhD told Live Science.email.
Shett and his team are organizing larger trials of CAR T-cell therapy for lupus, as well as the autoimmune diseases systemic sclerosis and myositis. In the future, the therapy could also be tested as a treatment for rheumatoid arthritis and multiple sclerosis, among other autoimmune diseases, Schett said.
If eventually approved, lupus CAR T “will be an option for patients with very severe SLE who have failed available therapies,” van Vollenhoven said. In the long term, the question is whether this new treatment can achieve long-term remission or even a ‘cure’. ”
“The potential for CAR T to reshape the immune system and lead to durable, treatment-free remission is exciting,” said Lin.
Originally published in Live Science.