Despite improved access to health insurance under the Affordable Care Act (ACA), breast cancer Mortality remains high, and the underutilization of advanced breast imaging may be one of the reasons, experts say.
In a recent position statement, researchers highlighted the disproportionately high breast cancer mortality rate among black women in Louisiana. 29.3 per 100,000 women, compared with
While Louisiana has made progress to improve access to breast cancer screening In recent years, the use of advanced imaging, especially breast MRI, has been underutilized in this high-risk population. A major barrier to widespread breast MRI adoption is cost, and expansion of the ACA has led to higher, rather than lower, out-of-pocket costs for this screening modality.
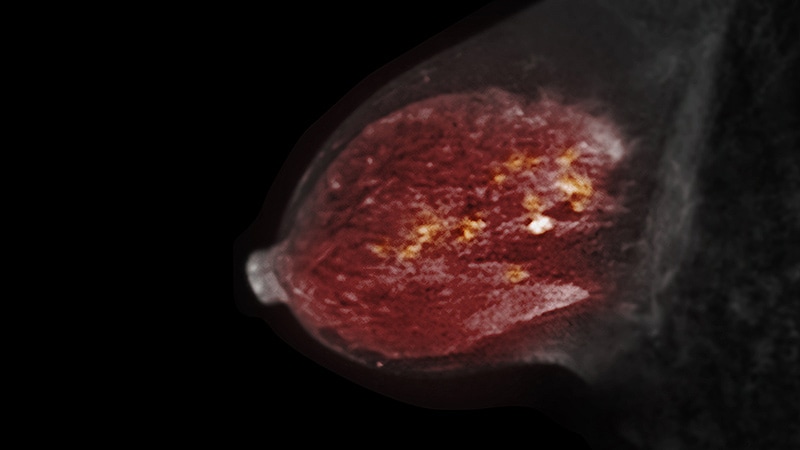
“Breast MRI is a powerful imaging tool for early detection of breast cancer and screening of women at high risk,” write the researchers, led by Brooke L. Morrell, M.D., Ph.D., of the Louisiana State University Health Sciences Center. .
However, increased access to health care has not necessarily led to increased breast MRI screening or improved survival among black women. Years after the adoption of the ACA, “black women in Louisiana continue to die from breast cancer at a rate well above the national average,” the authors write.
of Posted position statement early this month cancer.
Breast MRI is known to provide the highest breast cancer detection rates of any commonly used imaging option, with sensitivities ranging from 81% to 100%. This is approximately twice the sensitivity range. Mammography After considering breast density.
“This is particularly important when considering risk-based screening of younger populations, where dense breasts are more common,” the authors explain.
especially for black women Nearly a quarter (23%), according to the survey Those who develop breast cancer are diagnosed before age 50 compared to 16% of white women. Black women are also more likely to develop more aggressive premenopausal breast cancers, including triple-negative breast cancer, which are more easily detected on MRI.
“Adding adjunctive screening breast MRI to annual mammograms in high-risk women has been shown to detect up to 18 additional cancers in 1,000 patients,” Morrell said. . And “many of these cancers are detected much earlier than mammography alone.”
Yet, with the expansion of ACA, copayments for breast MRI have actually increased.This increase is partly due to the Women’s Preventive Services Guidelines It covers mammograms, but not breast MRIs.
More specifically, under the ACA, Medicaid and most private health insurance plans are required to provide free mammogram coverage to patients. The proportion of health insurance with zero-cost mammograms increased from 81.9% to 96.8% under the ACA, while the corresponding proportion of zero-cost breast MRI screening increased from 43.1% in 2009. It went backwards to just 26.2%. % 2017, a Research in 2022 found.
The study also highlighted geographic differences with no cost or out-of-pocket costs for breast MRI screening, with a higher financial burden observed for women living in the South. In addition, research has shown that racial and socioeconomic factors such as education and income play a role in the underutilization of screenings such as breast MRI.
All of these factors likely keep many women from being screened for breast MRI, Morrell and colleagues said.
The authors also outlined three key behavioral items to help address barriers to MRI breast screening.
-
Eliminate the high cost of breast MRI
-
Efforts to include breast MRI in ACA protection
-
Address knowledge gaps between patients and clinicians to better identify women who may benefit from breast MRI
On the financial side, the team explained that scan time for breast MRIs was a major contributor to the high costs. Simplified protocol.
“The widespread availability of low-cost shortened breast MRI screening could remove the cost barrier that adds breast MRI screening to ACA coverage without compromising diagnostic accuracy,” the authors noted. ing.
Further efforts should focus on overcoming cultural barriers, such as fear and mistrust of the healthcare system for black women. Outreach efforts may include public campaigns and town hall and church gatherings involving patient navigators, advocates, or community members.
“Our visibility in the community builds trust and gives us the opportunity to share knowledge that has the potential to empower women to become their own health advocates,” the authors wrote. increase.
Regarding the feasibility of revising the ACA policy to improve access and affordability of breast MRI, Morrell said: colon cancer sieving.
“Studies show that after the ACA changed policy, out-of-pocket costs for colonoscopies were reduced and screening Colonoscopy There has been a significant increase in the proportion of men, especially among socioeconomically disadvantaged people,” she noted. “Similarly, we will investigate how this applies to breast MRI screening.” is needed.
cancer. Published online on January 12, 2023. overview
Join us to learn more about Medscape Oncology twitter When Facebook