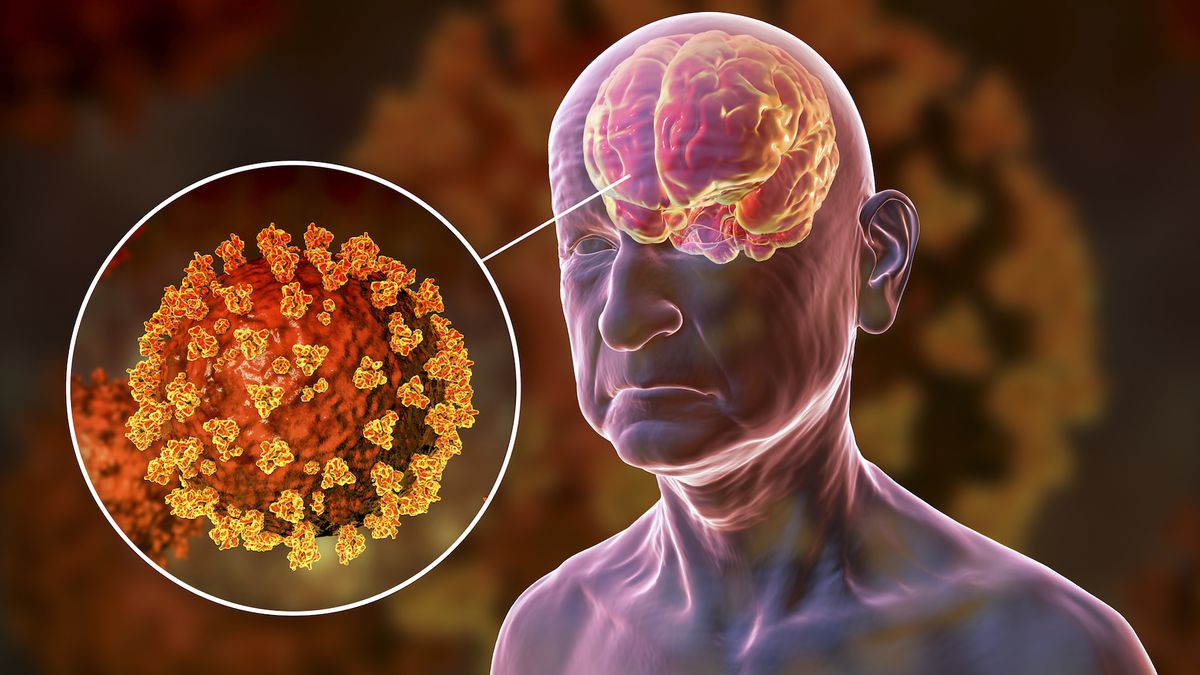
SARS-CoV-2, the virus that causes COVID-19, may preferentially use a “back door” into cells to infect the brain, a new mouse study suggests.
This discovery explains why so many Neurologic symptoms Fatigue, dizziness, Brain Fogor loss of smell or taste during or after a viral infection. Scientists believe these symptoms may occur during infection with SARS-CoV-2. Enters the central nervous systemHowever, how and why the virus moves from the respiratory tract to the brain has remained unclear until now.
Article published in the journal on August 23rd Nature MicrobiologyThe researchers: Viral spike proteinIt binds to this and enters human cells. A molecule called ACE2 It is located on the surface of the cell.
“The spike protein of SARS-CoV-2 coats the outside of the virus and enables it to enter cells,” said the study co-authors. Judd Hultquist“Typically, viruses can enter cells in two ways: through the cell surface (the front door) or from the inside after being internalized (the back door),” he, an assistant professor of infectious diseases at Northwestern University in Chicago, told Live Science in an email.
Part of the spike protein Furin cleavage sitehelps the virus get in through the front door. If this site mutates or is removed, the virus will only have the back door route available.
“Upper respiratory tract and lung cells are highly susceptible to SARS-CoV-2 infection, and SARS-CoV-2 can enter these cells through the front and back doors,” Hultquist said. “To reach the brain and replicate normally, the virus appears to need to enter through the back door. Deleting the furin cleavage site makes it more likely that the virus will use this pathway and thus more likely to infect brain cells.”
To study this, the researchers used genetically modified mice whose cells make human ACE2, infected them with SARS-CoV-2, then took virus samples from lung and brain tissue and sequenced the viral genome.
“We found that while we did see some infection in the brains of mice infected with regular SARS-CoV-2, when the virus had a mutation in the furin cleavage site, we saw much more infected cells,” Hultquist said. It remains to be seen whether these infected cells are the cause of COVID-19's neurological symptoms, but Hultquist and his colleagues observed a higher rate of infection in brain cells. Hippocampus The premotor cortex is associated with memory and movement, respectively.
However, this study was only conducted in mice, so further research is needed to explore whether similar requirements exist for SARS-CoV-2 to infect the human brain.
“It will be important to follow up this work with human samples to see if the same mutations seen in mice are also found in humans.” Matthew Freeman“As researchers target neuronal inflammation as a treatment for long COVID symptoms, it's crucial that we understand how the virus replicates in neurons in the first place,” a professor of microbiology and immunology at the University of Maryland who was not involved in the study told Live Science.
Hultquist also wants to learn more about why the furin cleavage site mutation makes it easier for the virus to enter the brain. “Studies have shown that normal SARS-CoV-2 can replicate in the brain when directly injected, suggesting that loss of the furin cleavage site is important for trafficking to the brain,” Hultquist said. “How this works remains a mystery.”
Nevertheless, the study could lay the groundwork for treating the neurological effects of COVID-19.
“If we know that the virus needs a back door to infect the brain, then we have a great opportunity to stop it from infecting the brain.” [it]”Small molecules that block this pathway may be particularly effective in preventing brain infection and its associated complications. The next challenge is to figure out not only which drugs are most effective, but also which ones can reach the brain,” Hultquist said.