With the new coronavirus burning all over the world, scientists are rushing to find ways to identify infected people, including those who have recovered from COVID-19. These people, if they think better, will not be affected by the deadly virus and could theoretically help them to resume their economy without fear of reinfection.
One of the key parts of this puzzle is developing what is called a serological test for specific antibodies in a person’s blood. So far, it has been used to estimate how much of the population is exposed in different regions such as New York City and Los Angeles.
But what are these tests? Also, is it really helpful in identifying those who are immune to SARS-CoV-2? Here’s everything you need to know about coronavirus antibody testing, from how they work to what they tell us.
Relation: COVID-19 Live Update
What is an antibody test?
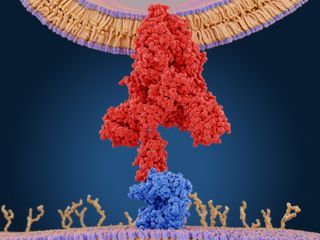
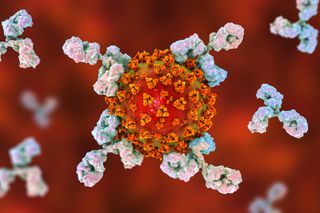
Outpatient intruders such as SARS-CoV-2 enter the body within a few hours, Immune system Performs non-specific attacks. That is, the body’s “common fighter” is thrown at the intruder. But eventually, the body begins to send out large Y-shaped molecules called antibodies that are targeted by the body Virus accurately. Antibodies bind to specific parts of the virus like a key.
Antibody tests are designed to detect these molecules.
“The purpose of the antibody test is not to ask if you’re feeling sick with COVID-19, but to see if a coronavirus has been detected in your immune system,” said assistant professor Daniel Larmor. University of Colorado Boulder Computer Science Department and BioFrontiers Institute.
Antibody tests are usually designed to detect one of two molecules, immunoglobulin M and immunoglobulin G. Within days to a week after the pathogen infects the body, the immune system produces small amounts of immunoglobulin M. Then, a few days to two weeks later, the body pumps out large amounts of immunoglobulin G. Previously reported live sciences. Because of the time it takes for this immune response to appear, antibody tests are negative in patients newly infected with COVID-19 and are not used for diagnosis.
“When it’s the beginning of an infection, you don’t pick it up, but only later,” said Dr Melanie Ott, a virologist and immunologist at the Gladstone Institute at the University of California, San Francisco. Told.
How does an antibody test work?
There are two types of antibody tests commonly used for testing SARS-CoV-2: lateral flow immunoassay and enzyme-linked immunosorbent assay (ELISA). Both use the same basic principles. A sample of human blood or serum (the liquid portion of blood) is washed with a surface that holds the molecules to which the antibody binds. When the antibody binds to these target molecules, the test is read by another chemical reaction, such as a color change.
“The lateral flow immunoassay is quick and easy for anyone to perform. It is basically similar to the stick pregnancy test in that it gives a visual reading (although blood or serum is used rather than pee). Very rapidly, “said Jesse Bloom, a virologist at Fred Hutchinson Cancer Research Center, in an email to Live Science.
The lateral flow assay is very easy to use and is easy to read, but it cannot be customized. On the other hand, ELISA testing should be done in the lab. It may use pipetting and plates and requires a technician to perform. Charlotte Sverkejogensen, who studies viral and microbiological special diagnostic serology at the Statens Serum Institute in Copenhagen, reported to Live Science that results typically take a few hours.
Each antibody test selects a specific part of the virus as the target molecule. For SARS-CoV-2, most tests Virus spike protein Used for invading cells. Several tests bind the S1 region of the coronavirus spike protein (the spike protein has two subunits, S1 and S2), Jorgensen said. Others bind to a small part of S1, called the receptor binding domain (RBD). This is a specific protein that enters the cell by latching on the human ACE2 receptor. Jorgensen said RBD could be the most specific part of the antibody to SARS-CoV-2, as other parts of the virus look like other coronaviruses.
Coronavirus Science and News
What makes antibody testing so good?
Generally, you need very sensitive and very specific tests. Highly sensitive means that the test will catch many people who are really infected with the virus. Specifically, there are few “false positives” or no one is positive even if they have never been exposed to SARS-CoV-2, both Bloom and Larmor said.
Currently, its false positive rate is particularly important. Most people in the United States are not exposed to SARS-CoV-2. In other words, false positives can dramatically distort the results. For example, if the test is 98% specific, 100 are virus positive, 98 are truly infected, and 2 of them have never been infected. It sounds good on paper, but if only 1% of the population is infected, you may find one who was truly positive and two who were falsely tested as positive. Most people who test positive were never infected, Blum told Live Science. The fewer viruses in the population, the more important the specificity is. (Recent antibody test results in Santa Clara and Los Angeles counties He is accused of having this problem. )
To ensure test specificity and sensitivity, manufacturers need to “calibrate” their tests. To do this, use blood or serum samples from people known to have COVID-19, and make sure that a high proportion of those people test positive with an antibody test. Conversely, to make sure that the test does not cause many false positives, you need to test the blood of people who are known to have no experience with COVID-19. It is unlikely that you will have been infected with the new coronavirus worldwide by the fall of last year, so ideally you need samples before that period, but not too old samples.
Like the produce in the grocery store, “I want a fresh, local blood sample,” Larmor said.
In this way, blood samples Coronavirus According to Larmor, the colds that cause the prevailing colds in the area during the season).
“We need to make sure that the tests don’t work when these coronaviruses are detected,” Larmor said.
The ELISA test can be tuned and fine-tuned for the local community using local samples. (Because different coronaviruses may have circulated in different regions, testing on a local sample will prevent the test from accidentally pinging the most common coronavirus in that region. I can). Do not customize. If the control sample used is from China, for example, we can detect the actual case of COVID-19, but we cannot rule out false positives. He added that misadjusted tests could overestimate the results of all kinds of community surveys inferring viral spread.
And as you can imagine, the more samples used to calibrate the test, the better the results. (Lamore has Built an online calculator Calibration data from a particular test can be used to predict sensitivity and specificity.
Does it mean you have immunity if you have antibodies?
Another tricky part of antibody testing is not knowing what it means for long-term or short-term immunity. Some people who broke COVID-19 do not produce antibodies at all, but they are not immune-free. For example, a study published in the preprint database on April 6 medRxivAlthough not peer-reviewed, it was found that out of 175 COVID-19 patients in China, approximately 30% (which tend to be younger) had very low antibody levels. It is also possible for the body to produce an antibody that is different from the antibody it gets in the test. That is, the test may be negative despite the immunity.
On the contrary, some people may develop antibodies, but those antibodies may not be very effective at neutralizing the virus, Ott said.
Other coronaviruses have a complex view of immunity. According to a 2017 study in the journal, people have produced antibodies to the more severe coronaviruses, SARS and MERS (Middle East respiratory syndrome) for at least several years Virus research. However, a coronavirus strain that causes a cold can reinfect the same person within a year, according to a peer-reviewed study, Published online by Columbia University. It is too early to say which camp SARS-CoV-2 falls into.
“In conclusion, if you make an antibody, you probably have some immunity, but I don’t know what will last for how long,” Ott told Live Science.
In other words, a reliable antibody test can estimate the number of people infected, but cannot tell individuals that they are immune to the disease.
Currently, a large amount of antibody tests are flooding the market. However, the results can be difficult to interpret because you don’t know the reliability of the results, Ott said.
“Science needs time to do things properly,” Ott said. “The virus hasn’t left us much time, but sometimes it doesn’t help rush something.”
Originally released Live science.