Health
Three-year outcomes of post-acute sequelae of COVID-19
There were 114,864 participants (13,810 (12.0%) females and 101,054 (88.0%) males) in the non-hospitalized COVID-19 group and 20,297 participants in the hospitalized COVID-19 group (1,177 (5.8%) females and 19,120 (94.2%) males), and there were 5,206,835 participants in the control group without infection (503,509 (9.7%) females and 4,703,326 (90.3%) males). All participants had a full 3 years of follow-up, totaling 344,592, 60,891 and 15,620,505 person-years of follow-up in the non-hospitalized COVID-19, hospitalized COVID-19 and control groups, respectively. Altogether, this corresponded to 16,025,988 person-years of follow-up. Demographic, health characteristics and standardized mean differences of the non-hospitalized COVID-19, hospitalized COVID-19 and control groups before and after inverse probability weighting for baseline covariates are presented in Supplementary Tables 1 and 2 and Extended Data Fig. 1.
We examined risks and burdens of death and a set of pre-specified PASC as well as sequelae aggregated by organ system and aggregated as an overall outcome of PASC by care setting during the acute phase of SARS-CoV-2 infection (non-hospitalized (n = 114,864) and hospitalized (n = 20,297) groups) in the first, second and third year after SARS-CoV-2 infection.
Risks in non-hospitalized participants
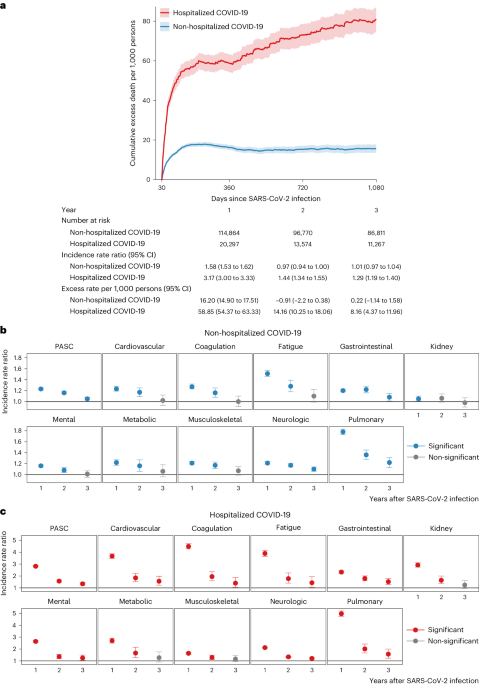
Compared to the control group without infection, people with COVID-19 who were not hospitalized during the acute phase of the disease were at an increased risk of death (incidence rate ratio (IRR): 1.58, 95% confidence interval (CI): 1.53–1.62; excess burden per 1,000 persons: 16.20, 95% CI: 14.90–17.51; Fig. 1a) during the first year after SARS-CoV-2 infection but not in the second year (IRR: 0.97, 95% CI: 0.94–1.00; excess burden per 1,000 persons: −0.91, 95% CI: −2.20 to 0.38) and third year (IRR: 1.01, 95% CI: 0.97–1.04; excess burden per 1,000 persons: 0.22, 95% CI: −1.14 to 1.58) after the infection.
a, The solid lines at the center of shaded bands were adjusted cumulative excess death rate per 1,000 persons in non-hospitalized COVID-19 (n = 114,864) and hospitalized COVID-19 (n = 20,297) groups compared to the control group without infection (n = 5,206,835), and the shaded bands present the 95% CIs for cumulative excess rates. The number at risk, weighted IRR and weighted excess rate per 1,000 persons in the COVID-19 groups by care setting of the acute phase compared to the control group without infection are also presented in the lower panel. b, IRR of overall PASC and by organ system in non-hospitalized COVID-19 group (n = 114,864) compared to the control group without infection (n = 5,206,835). The dots at the center of error bars in both panels represent the adjusted IRRs estimated using the number of post-acute sequelae, and the error bars correspond to the 95% CIs. c, IRR of overall PASC and by organ system in hospitalized COVID-19 group (n = 20,297) compared to the control group without infection (n = 5,206,835). Outcomes are ordered from top to bottom by largest cumulative number of post-acute sequelae at 3 years after infection in the non-hospitalized COVID-19 group. The dots at the center of error bars in both panels represent the adjusted IRRs estimated using the number of post-acute sequelae, and the error bars correspond to the 95% CIs.
The risks on the relative scale (IRRs) of PASC were 1.23 (95% CI: 1.22–1.25), 1.16 (1.14–1.18) and 1.05 (1.03–1.08) in the first, second and third year, respectively (Fig. 1b and Supplementary Table 3). The risks of individual outcomes in years 1, 2 and 3 are presented in Fig. 2, Supplementary Table 4 and Extended Data Fig. 2.
Heatmaps include non-hospitalized COVID-19 (n = 114,864; top rows) and hospitalized COVID-19 (n = 20,297; bottom rows) groups. IRRs were estimated in comparison to a control group without infection (n = 5,206,835). ACD, acute coronary disease; AKI, acute kidney injury; CKD, chronic kidney disease; DVT, deep vein thrombosis; ESRD, end-stage renal disease; GAD, general anxiety disorder; GERD, gastroesophageal reflux disease; IBS, irritable bowel syndrome; ICM, ischemic cardiomyopathy; ILD, interstitial lung disease; NA, not applicable; NCD, neurocognitive decline; NICM, non-ischemic cardiomyopathy; PTSD, post-traumatic stress disorder; TIA, transient ischemic attack; VTE, venous thromboembolism. If potential risk horizon (non-significant (NS) cell with a numeric IRR estimate) for an outcome was reached in a previous period, the IRRs for that outcome in all subsequent periods will not be estimated and are indicated by gray cells with NAs (not applicable) inside. yr, year.
The cumulative number of post-acute sequelae over the 3 years was 378.7 (95% CI: 356.6–401.1) per 1,000 persons, including 212.3 (197.5–227.0), 125.0 (107.2–142.7) and 41.2 (20.2–62.3) in the first, second and third year, respectively, which corresponded to 56.1% (52.2–60.0%), 33.0% (28.3–37.7%) and 10.9% (5.3–16.5%) of the total 3-year cumulative burden of PASC, respectively (Fig. 3 and Supplementary Table 3).
a, Number of post-acute sequelae overall and by organ system per 1,000 persons in the first, second and third year after SARS-CoV-2 infection by care setting of acute phase. b, Relative percentage of number of post-acute sequelae overall in the first, second and third year after SARS-CoV-2 infection by care setting of acute phase. Number of post-acute sequelae for COVID-19 not significantly different from the control group without infection in a year is marked by gray bars. The left column represents numbers of post-acute sequelae for the non-hospitalized COVID-19 group (n = 114,864), and the right column represents the numbers for the hospitalized COVID-19 group (n = 20,297), compared to the control group without infection (n = 5,206,835). Outcomes are ordered from top to bottom by cumulative number of post-acute sequelae at 3 years after infection.
The 3-year cumulative burden of DALYs due to PASC was 91.2 (95% CI: 81.6–101.0) per 1,000 persons, including 54.3 (47.9–60.7), 27.3 (19.5–35.0) and 9.6 (0.4–18.7) in the first, second and third year, respectively, which corresponded to 59.6% (52.5–66.6%), 29.9% (21.4–38.4%) and 10.5% (0.4–20.6%) of the total 3-year cumulative DALYs, respectively (Fig. 4 and Supplementary Table 3).
a, DALYs of overall PASC and by organ system per 1,000 persons in the first, second and third year after SARS-CoV-2 infection by care setting of acute phase. b, Relative percentage of DALYs of overall PASC in the first, second and third year after SARS-CoV-2 infection by care setting of acute phase. DALYs for COVID-19 not significantly different from the control group without infection in a year are marked by gray bars. The left panels of a and b represent the DALYs of post-acute sequelae for the non-hospitalized COVID-19 group (n = 114,864), and the right panels of a and b represent the number for the hospitalized COVID-19 group (n = 20,297), compared to the control group without infection (n = 5,206,835). Outcomes are ordered from top to bottom by cumulative DALYs of post-acute sequelae at 3 years after infection.
In the analyses for numbers of post-acute sequelae by organ system, the risks and burdens for each organ system in years 1, 2 and 3 for non-hospitalized group are provided in Figs. 1b and 3 and Supplementary Table 3. Compared to the control group without infection, there was increased risk for post-acute sequelae in all 10 organ systems in the first year; nine organ systems (all except kidney disorders) exhibited increased risks in the second year; and three organ systems exhibited increased risks in the third year, including neurologic, pulmonary and gastrointestinal disorders—contributing 14.2 (95% CI: 8.4–20.0), 11.1 (6.3–15.8) and 7.4 (0.8–13.9) sequelae per 1,000 persons in the third year, respectively. This corresponded to 7.2 (1.0–13.4), 1.5 (0.6–2.4) and 0.8 (0.02–1.5) DALYs in the third year for neurologic, pulmonary and gastrointestinal disorders, respectively (Fig. 4 and Supplementary Table 3). A Sankey plot showing the relative ranking of number of sequelae and DALYs by organ system in years 1, 2 and 3 is shown in Fig. 5a,b.
a, Changes of number of post-acute sequelae by organ system in 3 years after SARS-CoV-2 infection in the non-hospitalized COVID-19 group (n = 114,864). b, Changes of DALYs of post-acute sequelae by organ system in 3 years after SARS-CoV-2 infection in the non-hospitalized COVID-19 group (n = 114,864). c, Changes of number of post-acute sequelae by organ system in 3 years after SARS-CoV-2 infection in the hospitalized COVID-19 group (n = 20,297). d, Changes of DALYs of post-acute sequelae by organ system in 3 years after SARS-CoV-2 infection in the hospitalized COVID-19 group (n = 20,297). The height of each box represents the number of sequelae or DALYs in COVID-19 groups that are significantly different from the control group without infection in each year after SARS-CoV-2 infection. Outcomes are ordered from top to bottom by number/DALYs of post-acute sequelae per 1,000 persons in each year after SARS-CoV-2 infection in the COVID-19 group.
The 3-year cumulative number of sequelae and DALYs for each organ system are provided in Figs. 3 and 4, Supplementary Table 3 and Extended Data Figs. 3 and 4. Considering DALYs (Fig. 4), and in descending order, the top five organ systems were neurologic, cardiovascular, pulmonary, coagulation and hematologic and mental disorders. The 3-year cumulative number of sequelae per 1,000 persons was 79.5 (73.4–85.7) for neurologic, 33.0 (28.0–38.3) for cardiovascular, 66.7 (63.1–70.4) for pulmonary, 24.1 (20.5–27.9) for coagulation and hematologic and 56.9 (49.2–64.7) for mental disorders. The associated DALYs per 1,000 persons were 32.2 (27.5–37.1) for neurologic, 16.9 (13.4–20.5) for cardiovascular, 10.5 (9.8–11.1) for pulmonary, 9.7 (8.3–11.2) for coagulation and hematologic and 7.2 (4.7–9.8) for mental disorders.
Risks in hospitalized patients
Compared to the control group without infection, people with COVID-19 who were hospitalized during the acute phase of the disease were at an increased risk of death during the first year (IRR: 3.17, 95% CI: 3.00–3.33; excess burden per 1,000 persons: 58.85, 95% CI: 54.37–63.33; Fig. 1a), during the second year (IRR: 1.44, 95% CI: 1.34–1.55; excess burden per 1,000 persons: 14.16, 95% CI: 10.25–18.06) and during the third year (IRR: 1.29, 95% CI: 1.19–1.40; excess burden per 1,000 persons: 8.16, 95% CI: 4.37–11.96) after SARS-CoV-2 infection.
The risks on the relative scale (IRRs) for post-acute sequelae were 2.82 (95% CI: 2.76–2.89), 1.57 (1.49–1.66) and 1.34 (1.24–1.45) in the first, second and third year, respectively (Fig. 1c and Supplementary Table 5). The risks of individual outcomes in years 1, 2 and 3 are presented in Fig. 2, Supplementary Table 4 and Extended Data Fig. 2.
The cumulative number of post-acute sequelae over the 3 years was 2,391.7 (95% CI: 2,316.0–2,472.3) per 1,000 persons, including 1,696.6 (1,636.6–1,756.6), 443.3 (375.1–511.6) and 252.8 (176.9–328.7) in the first, second and third year, respectively, which corresponded to 70.9% (68.4–73.4%), 18.5% (15.7–21.4%) and 10.6% (7.4–13.7%) of the total 3-year cumulative burden of PASC, respectively (Fig. 3 and Supplementary Table 5).
The 3-year cumulative burden of DALYs due to PASC was 766.2 (95% CI: 731.7–803.3) per 1,000 persons, including 527.1 (499.5– 554.7), 149.6 (118.1–181.0) and 90.0 (55.2–124.8) in the first, second and third year, respectively, which corresponded to 68.8% (65.2–72.4%), 19.5% (15.4–23.6%) and 11.7% (7.2–16.3%) of the total 3-year cumulative DALYs, respectively (Fig. 4 and Supplementary Table 5).
In the analyses for the numbers of post-acute sequelae by organ system, the risks and burdens for each organ system in years 1, 2 and 3 for the hospitalized group are provided in Figs. 1c and 3 and Supplementary Table 5. Compared to the control group without infection, there was increased risk of post-acute sequelae in all 10 organ systems in the first and second year, and seven organ systems (except kidney, metabolic and musculoskeletal) exhibited increased risks in the third year—contributing 41.3 (14.1–68.4) sequelae for cardiovascular, 43.1 (6.2–80.1) for mental, 29.9 (19.3–40.6) for neurologic, 21.3 (0.3–42.2) for coagulation and hematologic, 28.7 (10.1–47.3) for pulmonary, 11.7 (0.2–23.2) for fatigue and 46.9 (24.1–69.8) for gastrointestinal disorders per 1,000 persons in the third year, respectively. This corresponded to 25.5 (7.4–43.6) DALYs for cardiovascular, 20.1 (7.3–33.0) for mental, 11.9 (0.1–23.8) for neurologic, 10.0 (1.1–18.8) for coagulation and hematologic, 4.8 (1.2–8.5) for pulmonary, 2.6 (0.1–5.2) for fatigue and 5.5 (2.8–8.2) for gastrointestinal disorders per 1,000 persons in the third year, respectively (Fig. 4 and Supplementary Table 5). A Sankey plot showing the relative ranking of number of sequelae and DALYs by organ system in years 1, 2 and 3 is shown in Fig. 5c,d.
The 3-year cumulative number of sequelae and DALYs for each organ system are provided in Figs. 3 and 4, Supplementary Table 5 and Extended Data Figs. 3 and 4. Considering DALYs (Fig. 4), and in descending order, the top five organ systems were cardiovascular, mental, neurologic, coagulation and hematologic and kidney disorders. The 3-year cumulative number of sequelae per 1,000 persons was 318.8 (299.5–339.7) for cardiovascular, 536.4 (510.1–564.6) for mental, 282.2 (263.6–302.2) for neurologic, 274.5 (259.7–290.5) for coagulation and hematologic and 197.0 (180.9–214.7) for kidney disorders. The associated DALYs per 1,000 persons were 173.5 (160.5–187.5) for cardiovascular, 156.3 (147.1–166.2) for mental, 138.5 (123.7–155.0) for neurologic, 107.5 (101.3–114.2) for coagulation and hematologic and 72.4 (66.7–78.7) for kidney disorders.
Risk in hospitalized versus non-hospitalized participants
Compared to those who were not hospitalized, people who were hospitalized during the acute phase of SARS-CoV-2 infection had significantly higher risk and burden of overall PASC and sequelae in every organ system at each timepoint (Fig. 6 and Supplementary Table 6) and longer risk horizons (Fig. 6 and Supplementary Table 6). The cumulative DALYs of the hospitalized people at 3 years (766.2 per 1,000 persons; 95% CI: 731.7–803.3) were 8.4 times higher than the non-hospitalized group (91.2 per 1,000 persons; 81.6–101.0) (Fig. 6 and Supplementary Table 6).
a, IRRs (95% CIs) of number of sequelae for hospitalized (n = 114,864) and non-hospitalized (n = 20,297) COVID-19 groups by year. IRRs were estimated in comparison to a control group without infection (n = 5,206,835). The dots at the center of error bars represent the adjusted IRRs estimated using the number of post-acute sequelae, and the error bars correspond to the 95% CIs. b, Number of sequelae per 1,000 persons due to SARS-CoV-2 infection in hospitalized and non-hospitalized COVID-19 groups by year. c, DALYs per 1,000 persons due to SARS-CoV-2 infection in hospitalized and non-hospitalized COVID-19 groups by year. d, Cumulative number of sequelae per 1,000 persons due to SARS-CoV-2 infection for hospitalized and non-hospitalized COVID-19 groups at 3 years. e, Cumulative DALYs per 1,000 persons due to SARS-CoV-2 infection for hospitalized and non-hospitalized COVID-19 groups at 3 years. a is ordered by the IRRs among the hospitalized COVID-19 groups in each year. The red and blue dots show the IRRs in hospitalized and non-hospitalized COVID-19 groups significantly larger than 1, and the error bars are the associated CIs. In b, c, d and e, the red dots represent the absolute rates in hospitalized COVID-19 groups significantly higher than those in the control group without infection; the blue dots represent the absolute rates in non-hospitalized COVID-19 groups significantly higher than the control group without infection; and the gray dots represent the absolute rates in hospitalized or non-hospitalized COVID-19 groups that were not significantly higher than those in the control group without infection. The thicker horizontal bars represent the excess rates in the hospitalized COVID-19 group compared to the non-hospitalized COVID-19 group, where the red bars indicate significantly different rates and gray bars indicate no statistical difference. The thinner horizontal bars closer to the y axis represent the absolute rate in the non-hospitalized COVID-19 group compared to the control group without infection. The organ systems in b, c, d and e were sorted based on the statistical significance and magnitude of differences between hospitalized and non-hospitalized COVID-19 groups (the horizontal red/gray bars between two dots).
Sensitivity analyses
We conducted several sensitivity analyses. (1) We built doubly robust adjustment models in which the covariates were used in both exposure and outcome models, instead of the primary approach where the covariates were applied only in the exposure model. (2) We constructed zero-inflated Poisson models instead of Poisson models in the primary approach. (3) We did not censor participants in the COVID-19 groups upon reinfection, whereas, in the primary approach, participants in the COVID-19 groups were censored upon reinfection. (4) We additionally adjusted for 100 algorithmically selected high-dimensional covariates, instead of only using a set of pre-specified covariates in our primary approach. (5) Instead of defining hospitalization during the acute phase as inpatient admission date within 7 d before or within 30 d after the positive test in the main analyses, we used an alternative definition of hospitalization as inpatient admission date on the day of the positive test or within 30 d after the positive test. (6) We truncated propensity score weights at 99.5% percentiles rather than the 99.9% percentiles in the main analyses. (7) We estimated the IRRs among a sample with complete data on all covariates (n = 4,432,414, 83.0% of the full sample) to test the consistency of the results with those obtained using multiple imputation for missing data. (8) We estimated the risks based on Fine–Gray models where death and SARS-CoV-2 infection during follow-up were considered as competing risks. (9) We applied inverse probability of censoring weight to account for non-random censoring due to death or SARS-CoV-2 infection during follow-up across the three groups (the control group without infection, the non-hospitalized COVID-19 group and the hospitalized COVID-19 group). (10) We alternatively used a narrower definition of PASC that included 73 outcomes instead of the 80 outcomes included in the primary analyses. The results from these sensitivity analyses are consistent with those from the main analyses (Supplementary Table 7).
Negative outcome control analyses
We examined the association between COVID-19 and incident neoplasm as a negative outcome control. The results suggested neutral associations between COVID-19 and the negative outcome control in non-hospitalized participants (IRRs of 1.03 (0.98–1.08) in the first year, 0.94 (0.87–1.01) in the second year and 0.95 (0.88–1.03) in the third year) and hospitalized patients (IRRs of 0.93 (0.82–1.05) in the first year, 0.92 (0.72–1.12) in the second year and 0.93 (0.68–1.08) in the third year).
|
Sources 2/ https://www.nature.com/articles/s41591-024-02987-8 The mention sources can contact us to remove/changing this article |
What Are The Main Benefits Of Comparing Car Insurance Quotes Online
LOS ANGELES, CA / ACCESSWIRE / June 24, 2020, / Compare-autoinsurance.Org has launched a new blog post that presents the main benefits of comparing multiple car insurance quotes. For more info and free online quotes, please visit https://compare-autoinsurance.Org/the-advantages-of-comparing-prices-with-car-insurance-quotes-online/ The modern society has numerous technological advantages. One important advantage is the speed at which information is sent and received. With the help of the internet, the shopping habits of many persons have drastically changed. The car insurance industry hasn't remained untouched by these changes. On the internet, drivers can compare insurance prices and find out which sellers have the best offers. View photos The advantages of comparing online car insurance quotes are the following: Online quotes can be obtained from anywhere and at any time. Unlike physical insurance agencies, websites don't have a specific schedule and they are available at any time. Drivers that have busy working schedules, can compare quotes from anywhere and at any time, even at midnight. Multiple choices. Almost all insurance providers, no matter if they are well-known brands or just local insurers, have an online presence. Online quotes will allow policyholders the chance to discover multiple insurance companies and check their prices. Drivers are no longer required to get quotes from just a few known insurance companies. Also, local and regional insurers can provide lower insurance rates for the same services. Accurate insurance estimates. Online quotes can only be accurate if the customers provide accurate and real info about their car models and driving history. Lying about past driving incidents can make the price estimates to be lower, but when dealing with an insurance company lying to them is useless. Usually, insurance companies will do research about a potential customer before granting him coverage. Online quotes can be sorted easily. Although drivers are recommended to not choose a policy just based on its price, drivers can easily sort quotes by insurance price. Using brokerage websites will allow drivers to get quotes from multiple insurers, thus making the comparison faster and easier. For additional info, money-saving tips, and free car insurance quotes, visit https://compare-autoinsurance.Org/ Compare-autoinsurance.Org is an online provider of life, home, health, and auto insurance quotes. This website is unique because it does not simply stick to one kind of insurance provider, but brings the clients the best deals from many different online insurance carriers. In this way, clients have access to offers from multiple carriers all in one place: this website. On this site, customers have access to quotes for insurance plans from various agencies, such as local or nationwide agencies, brand names insurance companies, etc. "Online quotes can easily help drivers obtain better car insurance deals. All they have to do is to complete an online form with accurate and real info, then compare prices", said Russell Rabichev, Marketing Director of Internet Marketing Company. CONTACT: Company Name: Internet Marketing CompanyPerson for contact Name: Gurgu CPhone Number: (818) 359-3898Email: [email protected]: https://compare-autoinsurance.Org/ SOURCE: Compare-autoinsurance.Org View source version on accesswire.Com:https://www.Accesswire.Com/595055/What-Are-The-Main-Benefits-Of-Comparing-Car-Insurance-Quotes-Online View photos
to request, modification Contact us at Here or [email protected]









