Two UK hospitals working together Donations after Cardiovascular Death (DCD) Heart Transplant Program For children.
Doctors behind the plan said the world’s first pediatric heart transplant technology, previously available only to adults, expanded the donor pool and increased the number of transplants for eligible children by 50%.
This program is a partnership with Great Ormond Street Hospital (GOSH). Royal Papworth Hospital (RPH), and NHS blood and transplants.
“Reviving” the mind
This procedure uses a portable organ perfusion system called the TransMedics Cardiac Organ Care System (OCS). This allows doctors to resuscitate the heart, administer medication, maintain a heartbeat outside the human body, and keep the heart healthy while being transported to the recipient’s patient.
Currently, it is the only medical device that can create DCD. Heart transplant Clinical reality.

Jen Baxter, Chief Nurse, Organ Search / RPH
Hearts treated in this way can also be transported over longer distances, giving health care professionals time to assess heart function and administer medication as needed.
Importantly, the DCD program can use cardiopulmonary criteria to recover organs for transplant from donors weighing 50 kg or more who have been diagnosed and confirmed to die with the consent of the donor’s family.
The partnership will include a team at RPH in Cambridge recovering the heart and another team at GOSH transplanting the organs.
Waiting time
Children are currently facing longer than average waiting times, as it is difficult to find a suitable match and the consent rate for pediatric organ donation is much lower than the national average for adults.
GOSH currently has 24 children waiting for a heart transplant. Between 2014 and 2019, the average waiting time was 282 days.
This technique is described as a “promising solution” to the shortage of children who can accept the adult heart.
Six pediatric heart transplants were performed in children aged 12 to 16 in 2020, and despite the COVID-19 pandemic, the total number of GOSH transplants increased to a record 24.
Work is underway to develop a new machine, mOrgan, that will allow the donation of DCD hearts from young children.
Regarding the program, Dr. Jacob Simmonds, a GOSH cardiologist and transplant doctor, said: Work is already underway to change the game to make this technology suitable for our much younger and smaller patients. “
Marius Bernan, a consultant for cardiothoracic transplant surgeons at Royal Papworth Hospital, said: Organ donation and recovery, transplant coordinator, doctor, surgeon.
“Above all, this is not possible without the generosity of all donors and their families.
“Really, it shows the best of the NHS and what can be achieved when we get together for the benefit of our patients.”
Anna’s story
The first child to undergo a DCD heart transplant under this plan was Anna Hadley, now 15 years old.
Anna was diagnosed in January 2018 Restrictive cardiomyopathy After collapsing during a PE class.Anna and her parents said she wouldn’t receive the heart in time Heart-lung transplant..
Towards the end of 2019, Dr. Simmons talked with Anna’s family about an upcoming transplant program already established for adults. Twenty months after being on the waiting list, Anna underwent surgery with the consent of her family.
Anna’s father said, “As a result of comparing the potential risks and benefits of DCD heart transplantation with conventional ones, I realized that I had only one option, and I was very happy to have it. Five days after the transplantation. Anna was walking up and down the hallway, chatting and giving high fives. It was incredible. “
Freyja’s story
Freya Heddington was 12 years old when she was also diagnosed with restrictive cardiomyopathy. So she was weak, short of breath, syncope..
She said, “I remember when they first taught me about my heart. I was scared because I didn’t know what that meant. I went to school, met friends, and now But can you do everything you like? Do you like riding horses?
“I knew that transplantation would be a major surgery, and that it was my best chance to get back to normal.”
Approximately six months after being listed for an emergency heart transplant, Freyja became the second child to undergo a heart transplant under the DCD program.
Regarding her surgery, Freyja said: “For me, it happened much earlier than most kids.
“I am very grateful to the donors and their families for giving me this second chance. When I woke up from surgery, I was finally able to breathe again.”
DCD Heart Transplantation for Adults
The DCD porting program will be available to adults from March 2015.
According to the Royal Papworth Hospital NHS Foundation Trust 48% increase in adult heart transplant activity in hospitals In 5 years.
In the five years following the breakthrough, the Royal Papworth Hospital recovery team was called in by 128 DCD cardiac donors, 79 of whom were eventually transplanted.
A 2020 treatise published Journal of Heart and Lung Transplantation The 30-day survival rate after DCD transplantation was 97%, compared to 99% with the unanimous donation of the Brainstem Death (DBD) group. Their one-year survival rate was 91%, compared to 89% in the DBD group.
The time spent on critical care was similar, with DCD recipients spending 7 days on critical care compared to 6 days for DBD recipients.
John Forsythe, Medical Director of Organ Donation and Transplantation at NHS Blood and Transplant, said: It wasn’t possible in the past and brought the patients on the waiting list to life.
“This new technology is an important step forward in heart transplantation in the United Kingdom and, in fact, elsewhere in the world.”
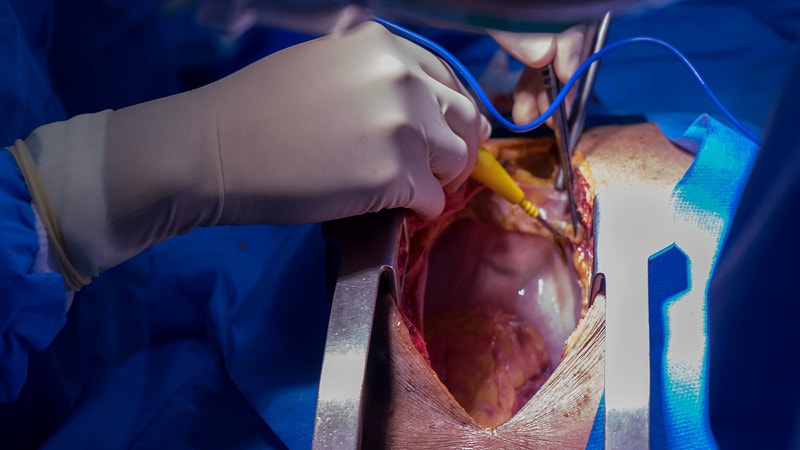
3/10 WARNING – GRAPHIC VIDEO
This is also known as a non-beating heart transplant.
After death, the donor heart is retrieved and put on the OCS, where it is kept warm and perfused with blood to mimic the human body, and reanimated.
This is what an adult DCD heart looks like: pic.twitter.com/nXvB5f9r3j
— Royal Papworth Hospital NHS FT ? (@RoyalPapworth) February 21, 2021