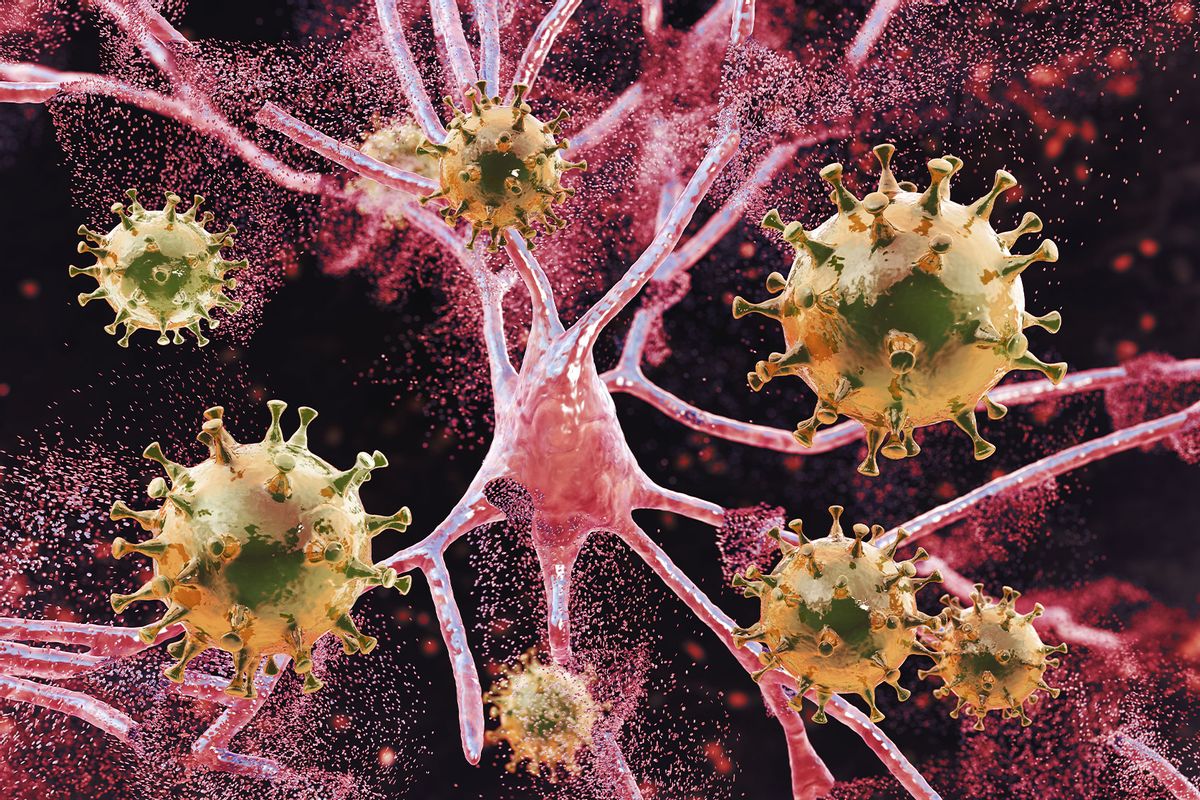
We usually think of SARS-CoV-2, the pathogen that causes COVID, as a respiratory virus. airborne, usually transmitted to humans through the nose or lungs, respiratory symptoms favorite cough When sore throatBut maybe we should start thinking of SARS-CoV-2 as a brain virus too.
After all, we have hard evidence SARS-2 can infect the brain, causing long-term or permanent damage. This can lead to life-threatening stroke or encephalitis, inflammation of the brain, or what is colloquially called.forgetfulness.”
Dysmia, even loss of taste and smell, was considered a characteristic symptom of the disease, it is changing -teeth neuropathy, a category of conditions that affect the brain and central nervous system. including stroke, epilepsy, Alzheimer’s disease, Parkinson’s disease, meningitis. Surprisingly, SARS-CoV-2 is all these neurological dysfunction When more.
SARS-CoV-2 appears to activate the same mechanisms in the brain that can cause brain disorders characterized by Parkinson’s disease, involuntary movements, tremors and balance disturbances.
Fortunately, developing these neurological conditions from COVID seems unusualThe tendency to develop such symptoms also depends on how severe the infection is or has been, and vaccinated people generally milder or temporary symptoms. Medical history can also affect the likelihood of developing neuropathy. However, age doesn’t seem to be a big factor. children may be affectedthat too.
We also do not know to what extent repeated infections may play a role in this condition, or whether certain virus variants are more susceptible to neurological damage than others.variant soup“Apparently set to ravage North America and Europe this winter, experts still have many questions about COVID and the brain, but what we are learning is not reassuring.
What we do know is that SARS-CoV-2 appears to activate the same mechanisms in the brain. Parkinson’s disease, a brain disorder characterized by involuntary movements, tremors, and balance disturbances.new research in the journal molecular psychiatry It shows for the first time that SARS-2 can trigger the same inflammatory process seen in Alzheimer’s and Parkinson’s patients.
Want more health and science articles in your inbox? Subscribe to the salon’s weekly newsletter a vulgar scientist.
The good news is that these researchers have identified a way to stop this process using drugs. So in the future, there may be pills to take to prevent brain damage from COVID. To find out how, an international team of researchers led by Professor Trent Woodruff of the University of Queensland conducted several different experiments, including mice, kidney cells from African green monkeys, and human immune cells called microglia. neuron.
In each of these experiments, scientists were looking for NLRP3A class of proteins called inflammasomes that protect the brain from attackers by releasing large amounts of inflammatory markers. NLRP3 has been extensively studied, with several studies guilty This protein against the root cause of Parkinson’s disease.
Dr. Albornoz Balmaceda describes this inflammatory cascade like a “fire” in the brain that cleans up and kills the neurons in its wake.
In each of these studies, whether in petri dishes or animal models, we found that NLRP3 was activated. That said, SARS-2 infection in the brain also appears to activate NLRP3, potentially increasing the risk of developing Parkinson’s disease or related neurological conditions.
“We studied the effects of the virus on the brain’s immune cells ‘microglia’, key cells involved in the progression of brain diseases such as Parkinson’s and Alzheimer’s,” said Professor Woodruff. statementWhen his team grew human microglia in the lab and infected these cells with SARS-2, they found signs of intense inflammation familiar to neuroscientists studying Parkinson’s disease. I was. “We found that it effectively makes the cell ‘angry’ and activates the inflammasome, the same pathway that proteins in Parkinson’s and Alzheimer’s disease can activate in disease,” Woodruff said. .
Dr. Albornoz Balmaceda, another author of the study, describes this inflammatory cascade like a “fire” in the brain that clears out and kills the neurons in its wake. It’s something of a silent killer, as it doesn’t show external symptoms for years.
Anger fire in the brain sounds bad, but this inflammation actually serves a purpose. It’s not an evolutionary mistake. When pathogens like viruses cross the blood-brain barrier, they form a shield around the brain to keep out unwanted substances, causing damage, infecting neurons and causing them to atrophy.
This triggers the release of NLRP3 and spreads more inflammatory proteins called caspases.These stop the spread of invaders, wipe out the damaged cells, and begin telling them to die in order to begin repair. pyroptosisThe Latin word “pyro” means fire, and the Greek word “ptosis” means falling like leaves. This type of inflammation can set off a chain reaction that kills many neurons like a series of firecracker bursts.
Some of this inflammation is natural and can be protected like controlled burns. As the neurons in the brain die, the brain begins to malfunction.
To further confirm this theory, the researchers repeated the experiment using drugs that block this pathway. The drug, obliquely called MCC950, stops NLRP3 signaling and Similar studies associated with this inflammatory pathway. MCC950 binds to her NLRP3, preventing inflammation and preventing the brain from essentially firing in anger.
Actually, the MCC950 is In development As a way to treat Parkinson’s disease, some studies in mice suggest that MCC950 may have side effects, such as kidney damage. However, there may be other similar drugs in the pipeline that block NLRP3, so hypothetically, such drugs could also block some of the harmful effects of SARS-CoV-2. I have. We now know at least one way SARS-CoV-2 could wreak havoc on the brain, but finding cures for SARS-CoV-2 and other neurological conditions such as Parkinson’s We are one step closer.