As reported, cases of monkeypox continue to grow — global aggregates 1 200 cases.. The Centers for Disease Control and Prevention (CDC) is competing to identify cases and tell you how to mitigate the spread of the virus. But in those efforts, experts say they unintentionally caused confusion.
Last week, the CDC Travel warning Advise the general public to “practice enhanced precautions,” such as washing hands and avoiding close contact with sick people. One of their recommendations was wearing a mask. “Wearing a mask helps protect you from many illnesses, including monkeypox,” the first notice said. A CDC spokesman said on Monday, June 6, the recommendation was removed because it “caused confusion.” statement To Reuters.

Dr. Monica Gandhi
The statement currently deleted is different from previous messages from the CDC and the World Health Organization (WHO). Both emphasized that the virus is transmitted primarily through close contact with people infected with monkeypox (such as skin-to-skin contact). The new travel advice from the CDC “made the infection seem to have been transmitted by accidental respiratory contact,” he said. Monica Gandhi, MD, MPHDeputy Chief of the Department HIVUniversity of California, San Francisco, Infectious Diseases, and Global Medicine, Medscape Medical News..
“The problem with that statement is that the mask can be interpreted as if it were a solution to prevent monkeypox infection, but this is not the case at all,” he added. Shira Doron, MD, Infectious disease specialist and hospital epidemiologist at Tufts Medical Center in Boston. “Masks will have little effect on monkeypox infections,” she said in an interview with Medscape.
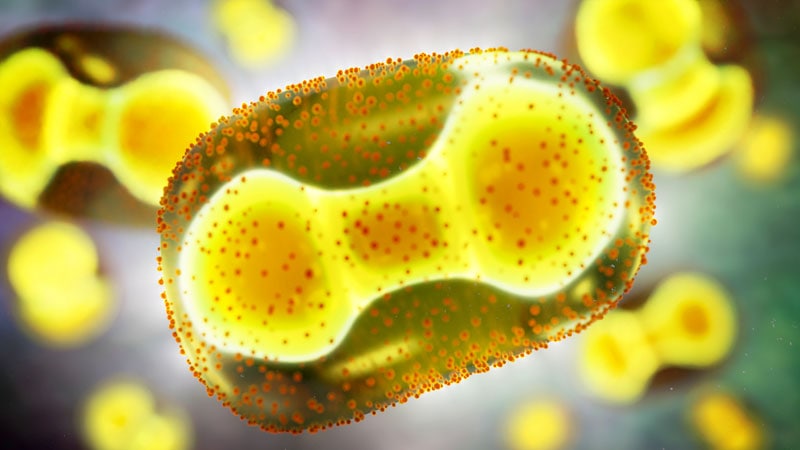
How monkeypox spreads
Monkeypox virus can be transmitted from person to person through monkeypox lesions, direct contact with the body fluids of an infected person, or from substances that come into contact with the virus, such as sheets and clothing. According to Gandhi, the virus can also spread from respiratory droplets from prolonged close face-to-face contact, such as kissing.
These respiratory droplets can also result from coughing and sneezing, neither of which is a symptom of monkeypox. However, Delon said this was not the primary means of infection in this current outbreak. “Based on the current epidemiology of this outbreak, it is almost exclusively present in men who have sex with men (MSM), and the virus is transmitted by close, long-term, skin-to-skin contact,” she said. Said. “If it was largely transmitted by the respiratory and aerial pathways, we would not see such a small proportion of infected individuals being female.”
No reported cases of monkeypox have been identified regarding gender, but the CDC said at a press conference on June 3 that only one of the 17 patients tested for monkeypox was a woman. Said. She had traveled to West Africa, where monkeypox is endemic, and reported that she was engaged in heterosexual sexual activity.
Researchers are still uncertain whether the virus can also spread through sexual intercourse or by close physical contact during sexual intercourse.
Including spread
There was also concern about the continued spread of the monkeypox virus and whether the virus could spread in one of the 29 countries that are not endemic but are currently reported. At a press conference on June 8, WHO Director General Tedros Adhanom Ghebreyesus, PhD, said the risk was “realistic” but “currently the most risky.”
WHO recommends contacting your healthcare provider if you have symptoms of monkeypox, such as a skin rash or lesion, or if you suspect that you have been in close contact with someone infected with the virus. Infected individuals should be quarantined until the lesion disappears, and individuals exposed to the virus at high risk should be quarantined for 21 days.
Gandhi and Delon seemed optimistic that they could contain the outbreak. “I don’t think it’s going to be an event like COVID,” Gandhi said. “Putting the public health department on top is absolutely careful and worrisome … but I’m not going to warn the general public.”
There is no evidence of asymptomatic or presymptomatic spread of monkeypox, “this is great news,” Delon said. “It’s probably very safe if you can avoid prolonged contact with people with symptoms.”
Nonetheless, Delon has access to tests to properly identify cases so that patients can isolate themselves and public health authorities can perform contact tracing to mitigate future spreads. He said it needed to be expanded. Currently, testing for the orthopox virus, a family of viruses to which the monkeypox virus belongs, is not performed in hospital laboratories, and such testing is performed only in 74 laboratories nationwide. STAT Report.
To request an Orthopox virus test, the doctor must call the state public health authorities to file a proceeding. Cases with suspected monkeypox usually, but not always, meet one of three criteria. Cases that identify the patient as having men who have sex with men, travel to the country where the patient occurred, or the patient is confirmed or suspected. The test cannot be conducted without state approval.
The bottleneck and restriction guidelines can miss cases of monkeypox, Delon said. “I want to quickly reach a point where we can broaden the standards of those who test,” she said. “I’m testing in a hospital lab and want to get to the point where I don’t need permission right away.”
Follow Medscape for more news. Facebook, twitter, InstagramWhen YouTube..