Health
Don’t Panic: Comprehensive Ars Technica Guide on Coronavirus [Updated 4/4]
![Don't Panic: Comprehensive Ars Technica Guide on Coronavirus [Updated 4/4]](https://i0.wp.com/cdn.arstechnica.net/wp-content/uploads/2020/03/covid19-explainer-starfield-800x450.jpg?resize=740%2C416&ssl=1)
Aurich Lawson / Getty
Approximately 1.2 million people have been infected with the new coronavirus, which has been widespread in the past few months since its outbreak in China. Almost 64,000 people have died. Here is a comprehensive guide to understanding and addressing this global public health threat.
This is a rapidly spreading epidemic and this guide will be updated regularly to provide as much preparation and information as possible.
March 8: First publication of document.
Latest Update April 4, 2020: Update added to section death, how Transmission Compares to Flu,and mask. Global and US cases Has also been updated.
A list of all updates and additions to this document is at the end.
table of contents
- How much should I worry?
- What is SARS-CoV-2?
- Where did SARS-CoV-2 come from?
- How did you start infecting people?
- What happens if I get infected with SARS-CoV-2?
- What are the symptoms?
- Does COVID-19 cause loss of smell? [New, 3/23/2020]
- How serious is the infection?
- Who is at risk of becoming the most seriously ill and dying?
- Are men at greater risk?
- Are your children at risk? [Updated 3/20/2020]
- Are pregnant women at high risk? [New, 3/19/2020]
- US data on millennials’ risks [New, 3/20/2020]
- How long will COVID-19 last?
- ⇒ How many people die from infection? [UPDATED 4/4/2020]
- How does COVID-19 compare to seasonal flu in terms of symptoms and death?
- How does SARS-CoV-2 spread? [Updated 3/12/2020]
- ⇒ How is coronavirus infection compared to influenza? [UPDATE 3/13/2020, 4/4/2020]
- Is it contagious? [New, 3/9/2020]
- Can I get SARS-CoV-2 from pets? Can I give it to my pet? [New, 3/9/2020]
- If I get COVID-19, will I be immune or re-infected? [Updated, 3/20/2020]
- How likely are you to get it in normal life?
- What can you do to prevent spread and protect yourself?
- Do I need a flu vaccine?
- ⇒ When do I need to buy or use a face mask? [UPDATE, 4/4/2020]
- Should we avoid large gatherings and trips? [Updated 3/13/2020]
- What precautions do I need to take when traveling?
- Can quarantine, quarantine, and social distance measurements help contain viruses? [New, 3/10/2020]
- How should we prepare for the worst scenario?
- Do I need to keep anything in the COVID-19 medicine cabinet? [Updated, 3/16/2020]
- Can a home remedy or product prevent, treat, or treat COVID-19? [New, 3/11/2020]
- Should I go to a doctor if I think I have COVID-19?
- When do I need emergency medical care?
- Is the US healthcare system ready for this?
- What are the test issues in the United States?
- ⇒Current litigation in the United States [Updated, 4/4/2020]
- What happens if a medical facility is overwhelmed?
- When does this all end in the United States?
- Does SARS-CoV-2 die in summer?
- Will it be a seasonal infection?
- What about treatment and vaccines?
- List of all updates and additions
How much should I worry?
You should worry and take this seriously. But don’t panic.
This is a mantra employed by public health professionals since the epidemic surge in January. This is as comfortable as it is easy to achieve. But it’s important that we all try.
This new coronavirus, called SARS-CoV-2, is definitely dangerous. This causes a disease called COVID-19, which is especially fatal for the elderly and those with underlying illness. The mortality rate of infected individuals is unknown, but even the current low estimates are seven times higher than those for seasonal flu.
And SARS-CoV-2 is here in the United States and is currently in circulation. We are just beginning to determine where it is and how far it has spread. Problems with federal testing have slowed the ability to detect traveler infections. And while we strive to catch up, the virus keeps moving. It seems that it has now spread to several communities across the country. It is unknown if it can be contained ahead of time. Even so, doing so requires a lot of resources and effort.
That said, SARS-CoV-2 is not a real threat. Although potentially fatal, about 80% of cases are mild to moderate and people recover in 1-2 weeks. In addition, there is a clear evidence-based action we can take to protect ourselves, our loved ones, and our entire community.
It is not time for panic. It only gets in the way of what you need to do. The worries are completely understandable, but the best way to get over this intactness is to pour that anxious energy to do what can be done to stop the spread of SARS-COV-2.
And to do that, you first need to get the most complete and accurate information about the situation. To that end, the following is the best attempt to address all questions about SARS-CoV-2, COVID-19, and the situation in the United States.
Start where all this starts, the virus itself.
What is SARS-CoV-2?
SARS-CoV-2 stands for Coronavirus 2 in severe acute respiratory syndrome. As the name implies, this is a coronavirus and is related to the causative coronavirus. SARS (Severe acute respiratory syndrome). Note: When SARS-CoV-2 is first identified 2019 Novel Coronavirus, or tentatively named 2019-nCoV.
Coronaviruses are a large family of viruses, derived from a halo of spiked proteins that decorate the outer surface under the microscope, resembling a crown (corona). As families, they infect a wide range of animals, including humans.
With the discovery of SARS-CoV-2, 7 types of coronavirus It is known to infect humans. Four circulate regularly in humans and mostly cause mild to moderate upper respiratory tract infections, essentially a cold.
The other three are coronaviruses, which have recently jumped from animal hosts to humans, causing more serious illness. This includes SARS-CoV-2, MERS-CoV causing Middle East Respiratory Syndrome (MERS), and SARS-CoV causing SARS.
In all three cases, the virus is thought to have passed from a bat carrying a large number of coronavirus strains to humans via an intermediate animal host. Researchers have linked SARS-CoV to the bat virus. Bats may have traveled to humans through masked palm civets and raccoon dogs sold for food at the live animal street market in China. MERS is thought to have spread from bats to dromedaries before jumping to humans.
Where did SARS-CoV-2 come from?
SARS-CoV-2 is associated with bat coronaviruses, but its intermediate animal host and human pathways have not yet been determined. There is a lot of speculation that the intermediate host may be a pangolin, It has not been confirmed.
How did you start infecting people?
Although the identity of the intermediate host of SARS-CoV-2 remains unknown, researchers have found that the mysterious animal is located in Wuhan, China, the heart of Hubei Province, a living animal market that is the epicenter of the outbreak. I suspect it existed. The market later described in the Chinese national media is “Dirty, dirtySells a variety of seafood and live animals, some of which are wild. Many of the first SARS-CoV-2 infections were market-related. In fact, many early cases were with the people who worked there.
Public health experts suspect that the market ambiguity has led to the spread of the virus. Such markets are notorious for promoting new outbreaks. They tend to crawl humans along with a variety of live animals that have their own pathogen breeding. Neighborhood, meat preparation and poor hygiene all offer so many opportunities to reassociate, mutate, and leap to new hosts, including humans
It said, Lancet Report Explaining the first 41 cases of outbreaks, the earliest identified individuals who became ill with SARS-CoV-2 were not relevant to the market. Ars as previously reported, The case was a male case that began to cause infection on December 1, 2019. None of the male families became ill, and he had no connection to any other cases of the outbreak.
The significance of this and the ultimate cause of its occurrence remain unknown.
On January 1, Chinese authorities closed and sanitized the market as the outbreak began to spread.
What happens if I get infected with SARS-CoV-2?
In humans, SARS-CoV-2 causes disease Dubbed COVID-19 According to the World Health Organization (WHO). As the US Centers for Disease Control and Prevention (CDC) points out, “CO” for “Corona”, “VI” for “Virus”, and “D” for Disease.
What are the symptoms?
COVID-19 is a disease with a variety of symptoms and severity, and we are still learning the full spectrum. So far, it appears to range from mild or potentially asymptomatic cases to moderate pneumonia, severe pneumonia, respiratory distress, organ failure, and even death.
It often begins with mild respiratory symptoms such as fever, malaise, and dry cough. In most cases, it does not worsen, but in some cases it can progress to serious illness.
According to data from approximately 56,000 COVID-19 patients confirmed by Chinese laboratory tests, the details of common symptoms are as follows:
- 88% have fever
- 68% had a dry cough
- 38% tired
- 33% coughed sputum
- 19% had shortness of breath
- 15% had joint or muscle pain
- 14% sore throat
- 14% headache
- 11% chills
- 5% had nausea or vomiting
- 5% stuffy nose
- 4% had diarrhea
- Mucus of blood or blood stain of less than 1%
- Less than 1% had teary eyes
The data is Report by an international band of health professionals gathered by WHO and Chinese authorities (Referred to as the WHO-China Joint Mission) visited the country for several weeks in February to evaluate the outbreak and response efforts.
Does COVID-19 cause loss of smell? [New, 3/23/2020]
There are case reports that many people who have COVID-19 or test positive for their illness have temporarily lost their sense of smell and their taste has declined.
There is not enough data on this. At a press conference on March 23, WHO also heard of these reports and stated that it was investigating data to see if this was a common symptom of COVID-19. Was.
However, the epidemiologist Maria Wankelhof, an outbreak expert at WHO, said that the main symptoms and severe forms of the disease, fever, cough, and fatigue, no matter whether loss of odor sensation was common or not Emphasis on knowing, shortness of breath.
How serious is the infection?
Most infected people become mildly ill and recover fully in two weeks.
In 44,672 confirmed epidemiological studies in China, prepared by an emergency response team of epidemiologists and published by the Chinese CDC, researchers 81% of cases were considered mild. Researchers defined mild cases as cases ranging from mild symptoms to mild pneumonia. None of the minor cases were fatal. All recovered.
Otherwise, approximately 14% were considered severe and were defined as having difficulty or difficulty breathing, increased respiratory rate, and decreased blood oxygen levels. None of the severe cases were fatal. All recovered.
Nearly 5% of cases were considered critical. These cases included respiratory failure, septic shock, and / or multiple organ failure or failure. About half of these patients died.
Finally, 257 patients (0.6%) had no severity data.
The overall mortality of the patients examined was 2.3%.
Who is at risk of becoming the most seriously ill and dying?
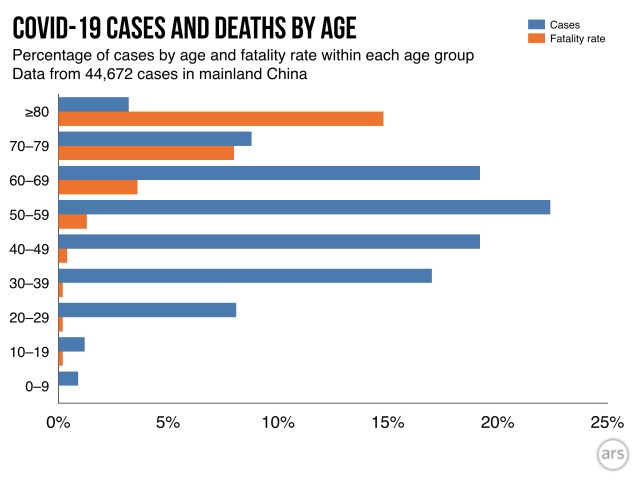
The risk of serious illness and death increases with age and underlying illness.
Of the 44,672 groups listed above, the highest mortality rates occurred in people over the age of 60. The death rate for people aged 60 to 69 was 3.6%. The mortality rate for the 70-79 age group was about 8%, and the mortality rate for the 80+ age group was about 15%.
In addition, researchers had information about other health conditions in 20,812 of the 44,672 patients. Of the people with additional medical information available, 15,536 said they had no underlying health condition. The mortality rate for that group was 0.9%.
The mortality rate of the remaining 5,279 patients who reported some underlying health conditions was much higher. The mortality rate for those who reported cardiovascular disease was 10.5%. Diabetes mortality was 7.3%. The proportion of patients with chronic respiratory disease was 6.3%. Hypertension patients had a mortality rate of 6.0% and cancer patients had a mortality rate of 5.6%.
Curiously, the mortality rate for men was higher than for women. In this study, 2.8% of adult male patients died, compared to 1.7% of female patients.
Are men at greater risk?
In several studies, researchers point out that men have more cases than women. The WHO Joint Mission Report found that men accounted for 51% of cases. Another study of 1,099 patients found that men 58% of cases.
So far, it is unclear whether these numbers are true or whether they will be even if the researchers looked at more cases. It is also unclear whether this bias reflects differences in exposure rates, underlying health, or smoking rates that may increase male susceptibility.
Nevertheless, there are gender differences in diseases caused by SARS-CoV-2 relatives, SARS-CoV and MERS-CoV. There are preliminary studies examining this in mice. In some findings, Protective effect of female hormones from estrogen activity. Suggests other studies Gene on X chromosome Viruses involved in regulating the immune response to the virus also help protect genetic women with two X chromosomes compared to genetic men with only one X chromosome.
Are your children at risk? [Updated 3/20/2020]
Yes, it is. In all previous studies and data, children account for only a small percentage of cases and few deaths have been reported. In 44,672 cases surveyed by the Chinese CDC, less than 1% of children were aged 0-9. None of those cases were fatal. Similar findings have been reported Other studies.
The WHO-China Joint Envoy report also wrote that in this epidemic children seemed almost intact and “children’s illness appears to be relatively rare and mild.” From previous data, they report that “infected children have been identified primarily by contact tracing in adult households.”
391 unpublished, unpeer reviewed studies in Shenzhen, China, seem to support that observation. It is a household Children seemed as likely to be infected as adults, But they had a milder case. The study was posted on the medical preprint server on March 4.
Nevertheless, as the Joint Mission report stated, given the data available, it is not possible to determine the extent of child infection and its role in promoting disease spread and pandemic. Is possible. The “Notable” report continued, “People interviewed by the joint mission team could not recall episodes where transmission from children to adults occurred.”
UPDATE 3/20/2020:
New data on the little children’s cases, little changed. Children still seem to be at low risk for COVID-19. They can indeed be infected, but in some places they tend to make up a small fraction of known cases. When infected, the disease becomes mild and rarely severe. To date, there have been few reports of children dying from COVID-19. The first was a 14-year-old boy living in Hubei, China, who died on February 7.
Surveys appeared in journal Pediatrics this week 2,143 COVID-19 in Chinese children. This study is often the first to examine in detail cases where it is difficult to find details.
Overall, it reflects what we already know. “The clinical symptoms of COVID-19 in children were milder than those in adult patients,” the authors concluded. About 94% of cases were mild or moderate.
But, like other demographics, children could not escape universally severe consequences. About 6% of cases were severe (about 5%) or serious (less than 1%). And, perhaps most worrisome, the most severe and serious cases were the youngest age group, under 1 and 1-5 years.
These two groups accounted for 60% of severe cases (about 30% each) and nearly 70 serious cases (54% for those under one year of age).
While these numbers are alarming, it is important to note some limitations of this data. First, there are few in serious and important categories. The percentage can be large in a few cases. For example, there were only seven serious cases of children under one year old, but only 13 in total.
Also, not all cases in this study were confirmed as COVID-19 cases. Some were suspected based on clinical findings. Of the 2,143 patients, 731 (34%) were laboratory confirmed and 1412 (66%) were suspected. Therefore, other respiratory infections, such as RSV, that can be particularly severe for infants cannot be ruled out.
Finally, the researchers did not have information about the child’s overall health. It is unknown whether the underlying condition contributed to the severity of the condition.
Are pregnant women at high risk? [New, 3/19/2020]
Unfortunately, the risk issue for pregnant women is very difficult to answer at this time. I just don’t have enough data.
So far, from the scarce data we have, there are few indications that pregnant women are at high risk for COVID-19. In other words, pregnant women do not seem to be more seriously ill than the rest of the population. At this time, no deaths of pregnant women due to COVID-19 have been reported.
However, pregnant women are at increased risk of becoming severely ill or dying Other Respiratory infections such as influenza and influenza SARS (This is caused by SARS-CoV, a coronavirus associated with SARS-CoV-2, the virus that causes COVID-19). For this reason, the American College of Obstetrics and Gynecology (ACOG) is currently (as of March 19) Recommendations to consider pregnant women as at-risk population.
US Centers for Disease Control and Prevention And Other health agencies Pregnant women emphasize the need to adhere to the same hygiene measures and social distances recommended to prevent transmission of the virus.
Here’s what we know if a pregnant woman gets the virus:
Pregnant women:
As in other populations, symptoms are more likely to be mild to moderate. However, severe symptoms can occur, especially if there is an underlying condition, and must be identified and treated promptly.
An unpublished, unpeer-reviewed study of 34 pregnant women with COVID-19 (Identified in 16 laboratories and 18 suspected cases), no women developed severe illness. Although women had a higher incidence of maternal complications than controls, all complications occurred before COVID-19 cases. These complications included gestational diabetes, premature rupture of the membrane, and preeclampsia.
Be Pregnant women reporting severe illness. She was hospitalized at week 34 and received an emergency C-section of a stillborn baby before being transferred to an ICU with multiple organ failure and acute respiratory distress syndrome.
For a fetus:
There is no evidence that the risk of miscarriage or early pregnancy loss is high.
There are reports of premature birth, but it is unknown at this time whether the premature birth was due to the mother’s COVID-19.
There is no evidence that the virus is transmitted in utero. In one small studyLaboratory-confirmed samples of amniotic fluid, cord blood, neonatal pharyngeal swabs, and breast milk from six pregnant women in cases of COVID-19 were all negative for SARS-CoV-2. In another study, Three placentas from pregnant women with COVID-19 were also negative. And Other researchFrom a newborn Symptomatic mother Negative virus test.
There are several reports that newborns are virus-positive, but the time of infection is unknown. It may have been infected shortly after birth.
In expert opinion, there is no intrauterine fetal infection. Therefore, it is unlikely that maternal COVID-19 will have a congenital effect on the fetus from SARS-CoV-2.
US data on millennials’ risks [New, 3/20/2020]
At a press conference on March 18, Dr. Deborah Birx, coordinator of the White House Coronavirus Control Headquarters, Send alerts to millennials—People in their twenties and thirties—not affected by the severity of COVID-19. In reports of youth illness in France and Italy, she said she did not take pandemic risk seriously, possibly because of an imbalanced infection. (Here are some Recent data on infections in Italy)
“We believe that, in part, listening to early data from China and South Korea has put the elderly and those with existing medical conditions at particular risk.” she said. “It may have been a millennial … there may be an unbalanced number of infections between the groups, and even if it were a rare event, it would be more It is often seen and may now be obvious. “
Her main point is that millennials are indeed very sick-although at a lower rate than the elderly group-they are certainly recommended health measures like the elderly And you need to keep social distance. But one might say that millennials in the United States are sicker than expected.
On the same day that CDC commented on Dr. Birx, Preliminary Data on Serious Outcomes of COVID-19 Patients in the United States. The data may provide eye-opening insights, but it is not much different from what you see elsewhere.
Overall, the data reflects what was seen in other countries, especially China. Patch data from 4,226 U.S. COVID-19 cases suggest that people aged 65 and over are at most risk, accounting for 31% of the population, despite being about 15% of the population You. They accounted for 45% of known hospitalizations, 53% of known ICU hospitalizations, and 80% of deaths. The age group with the highest rate of serious outcomes was the group aged 85 and older.
However, the data used by the CDC was very preliminary and incomplete. In many cases, researchers did not have data on age, such as whether hospitalization or intensive care was needed or whether the patient died. The data also did not include information on whether the patient had a serious illness, such as cardiovascular disease or diabetes, or an underlying condition that increased the risk of death.
Still, some of that data was finely divided. Of the 2,449 cases of known age, 29% were classified in the 20-44 year old group. Of the 508 patients hospitalized, 20% were between the ages of 20 and 44. Of 121 patients known to require intensive care, 12% were 20-44.
Finally, of the 44 known results, 9 (20%) were between the ages of 20 and 64.
The CDC finding that 20% of people hospitalized at COVID-19 are 20-44 years old may seem high. British researchers say one unpublished peer-reviewed study found that people aged 20-49 COVID-19の入院を必要とする人々のわずか約9%増加.推定値は、中国の3,665人のCOVID-19症例のデータに基づいています。
ただし、中国のデータを詳しく見ても、米国でこれまでに聞いた話とまったく異なる話にはなりません。 3,665人の中国の症例のうち、1,170人は20〜49歳でした。そのうち173人は重症で入院が必要と思われた。これは、20〜49歳のCOVID-19患者の約15%が入院を必要としていることを示唆しています。
米国のCOVID-19データに関する新しいレポートでは、CDCは20〜44歳の患者の14〜20%が入院を必要とすると推定しています。
もちろん、人口統計、疾病伝播ダイナミクス、ヘルスケアの質などが異なる場所では、これらのタイプの数値は変動します。たとえば、北京だけで262件のCOVID-19症例を調べたある研究では、研究者は 重度の症例の20%は13歳から44歳の人でした.
肝心な点は、65歳以上の人々と基礎疾患を持つ人々は、明らかに、最も深刻な病気を発症し、COVID-19で死ぬリスクがあるということです。しかし、より若い年齢層の人々は確かにそれらの結果の影響を受けません。
WHOのTedros局長は、3月20日の記者会見でミレニアル世代へのこのメッセージを強調しました。
そして、たとえ若いCOVID-19のケースが軽度の病気でうまくいったとしても、彼らは感染をより脆弱なグループに引き継ぐ可能性をまだ持っています。
誰もが、年齢や健康状態に関係なく、衛生および社会的距離の推奨事項に従う必要があります。全員。
COVID-19はどのくらい持続しますか?
平均して、SARS-CoV-2に感染した日からCOVID-19の症状が現れるまで、5〜6日かかります。この発症前の期間は、「潜伏期」とも呼ばれ、1〜14日間の範囲です。
そこから、軽度の疾患の患者は約2週間で回復する傾向がありますが、より重い症例の患者は回復するのに3〜6週間かかる場合がありますと、テドロス博士のそばにいるWEDのTedros Adhanom Ghebreyesus博士は述べています。
⇒何人が感染症で死亡しますか? [UPDATED 4/4/2020]
これは答えるのが難しい質問です。肝心なことは、私たちは本当に知らないということです。
致死率(CFR)、つまり感染により死亡する感染者の数は、死亡数を回復数と死亡数で割ることによって単純に計算されます。これまでに見たCFRは、これの大まかなバージョンである可能性があります。死亡数を総症例数で割ったものです。
これらの粗雑な計算の1つの問題は、カウントしているケースがすべて解決されないことです。現在病気になっている患者の一部は、後に死亡する可能性があります。その状況では、患者の症例は数えられますが、彼らの死は(まだ)数えられていません。これにより、現在の計算が歪められ、CFRが人為的に低く見えるようになります。
しかし、もっと大きな懸念は、全体としてのケース数を過小評価していることです。 COVID-19ケースのほとんどは 私たちが知っていること 軽度であり、より多くの感染者が検査を受けるために医療提供者に身を見せていなかったと健康専門家は疑っています。彼らはCOVID-19のケースを一般的な風邪と間違えたか、まったく気づかなかった可能性があります。 COVID-19の影響が大きい地域では、すべての軽度のケースを検出するのに十分なテスト能力がなかった可能性があります。総ケース数で多数の軽度のケースが見逃されている場合、CFRが人為的に高く見える可能性があります。
この不確実性を解消する最良の方法は、地域での集団発生の1つが完全に終わるまで待ってから、一般住民に対して血液検査を実施して、感染した人の数を確認することです。これらの血液検査は、SARS-CoV-2を標的とする抗体を探します。 (抗体とは、免疫系が病原体やその他の不親切な侵入者を特定して攻撃するのを助けるために作成するY字型のタンパク質です。)人の血液中の特定の細菌に対する抗体の存在は、感染によって、その細菌に人がさらされたことを示しますまたは予防接種。 SARS-CoV-2抗体の一般集団をスクリーニングすることで、症状があるか病気であるかを問わず、実際に感染した人の数をより明確に把握できます。その後、その数値を使用して正確なCFRを計算できます。
これまでのところ、中国、特に広東省でCOVID-19感染の予備的集団スクリーニングが行われています。発熱クリニックに通院した32万人をスクリーニングしたところ、膨大な数の軽度の症例を見逃していない可能性があることが示唆されました。これは、今計算しているCFRが本来あるべき値よりも大幅に高くなっていないことを示しています。しかし、専門家は、多くの軽度の症例が報告されないままであると依然として疑っていて、真のCFRが現在計算しているものよりも低くなると多くの人が予想しています。
CFRは、基本的なケース数と死亡数を正しく把握するだけでなく、人口、時間、場所によって異なるため、注意が必要です。すでに述べたように、CFRは年齢、性別、基礎となる健康に基づいて患者集団で増加します。しかし、時間が経つにつれ、医療提供者は患者の特定と治療において集合的に改善し、それによってCFRが低下します。
これらの統計をさらに複雑にし、ヘルスケアの質は場所によって異なります。リソースの少ない病院のCFRは、リソースの豊富な病院のCFRよりも高い場合があります。さらに、アウトブレイクで圧倒された医療システムは、すべての患者に最適なケアを提供できず、それらの場所のCFRを人為的に増加させる可能性があります。
これは、これまで中国で見られたもののようです。 WHOと中国の共同ミッションの報告で、専門家は武漢で、発生が始まった場所と、医療システムが事件の数によって押しつぶされた場所で、CFRがなんと5.8%だったと述べました。 The rest of China at the time had a CFR of 0.7 percent.
As of March 5, there were about 13,000 cases and 400 deaths reported outside of China’s Hubei Province (where Wuhan is located). A crude calculation puts the CFR around 3 percent, but this calculation will likely drift throughout the outbreak. We will update the current crude CFR periodically.
UPDATE 4/4/2020
As of April 4, there were 290,606 cases and 7,826 deaths in the US. A crude estimate puts the CFR at about 2.7 percent. In Italy and Spain, which have had devastating outbreaks, crude estimates of the CFRs are 12 percent and 9 percent, respectively.
What Are The Main Benefits Of Comparing Car Insurance Quotes Online
LOS ANGELES, CA / ACCESSWIRE / June 24, 2020, / Compare-autoinsurance.Org has launched a new blog post that presents the main benefits of comparing multiple car insurance quotes. For more info and free online quotes, please visit https://compare-autoinsurance.Org/the-advantages-of-comparing-prices-with-car-insurance-quotes-online/ The modern society has numerous technological advantages. One important advantage is the speed at which information is sent and received. With the help of the internet, the shopping habits of many persons have drastically changed. The car insurance industry hasn't remained untouched by these changes. On the internet, drivers can compare insurance prices and find out which sellers have the best offers. View photos The advantages of comparing online car insurance quotes are the following: Online quotes can be obtained from anywhere and at any time. Unlike physical insurance agencies, websites don't have a specific schedule and they are available at any time. Drivers that have busy working schedules, can compare quotes from anywhere and at any time, even at midnight. Multiple choices. Almost all insurance providers, no matter if they are well-known brands or just local insurers, have an online presence. Online quotes will allow policyholders the chance to discover multiple insurance companies and check their prices. Drivers are no longer required to get quotes from just a few known insurance companies. Also, local and regional insurers can provide lower insurance rates for the same services. Accurate insurance estimates. Online quotes can only be accurate if the customers provide accurate and real info about their car models and driving history. Lying about past driving incidents can make the price estimates to be lower, but when dealing with an insurance company lying to them is useless. Usually, insurance companies will do research about a potential customer before granting him coverage. Online quotes can be sorted easily. Although drivers are recommended to not choose a policy just based on its price, drivers can easily sort quotes by insurance price. Using brokerage websites will allow drivers to get quotes from multiple insurers, thus making the comparison faster and easier. For additional info, money-saving tips, and free car insurance quotes, visit https://compare-autoinsurance.Org/ Compare-autoinsurance.Org is an online provider of life, home, health, and auto insurance quotes. This website is unique because it does not simply stick to one kind of insurance provider, but brings the clients the best deals from many different online insurance carriers. In this way, clients have access to offers from multiple carriers all in one place: this website. On this site, customers have access to quotes for insurance plans from various agencies, such as local or nationwide agencies, brand names insurance companies, etc. "Online quotes can easily help drivers obtain better car insurance deals. All they have to do is to complete an online form with accurate and real info, then compare prices", said Russell Rabichev, Marketing Director of Internet Marketing Company. CONTACT: Company Name: Internet Marketing CompanyPerson for contact Name: Gurgu CPhone Number: (818) 359-3898Email: cgurgu@internetmarketingcompany.BizWebsite: https://compare-autoinsurance.Org/ SOURCE: Compare-autoinsurance.Org View source version on accesswire.Com:https://www.Accesswire.Com/595055/What-Are-The-Main-Benefits-Of-Comparing-Car-Insurance-Quotes-Online View photos
Pictures Credit
to request, modification Contact us at Here or collaboration@support.exbulletin.com



